Fellow Désirée Vandenberghe obtained a PhD in (health) economics in 2020, with her thesis entitled The economics of preventive healthcare. In it, she examined the challenges and opportunities of preventive healthcare within the context of chronic diseases. In this blog, Désirée outlines the importance of preventive and integrated care, illustrated by some great examples in Belgium.
When we talk about healthcare, we usually refer to the curative part of our care. This part carries - as its name suggests - care for people who are already ill or have a condition. However, these diseases and patients are only the tip of the so-called 'disease iceberg'. This iceberg is a metaphor for the entire spectrum between health and illness [1] (see figure). It illustrates that for every sick person, there is an even larger group that is at a stage between health and illness. Below the surface, the iceberg is made up of a large group of asymptomatic diseases and exposure to numerous risk factors. Examples of these risk factors are exhaust fumes or other pollutants. Together, they form the preliminary stage of actual disease.
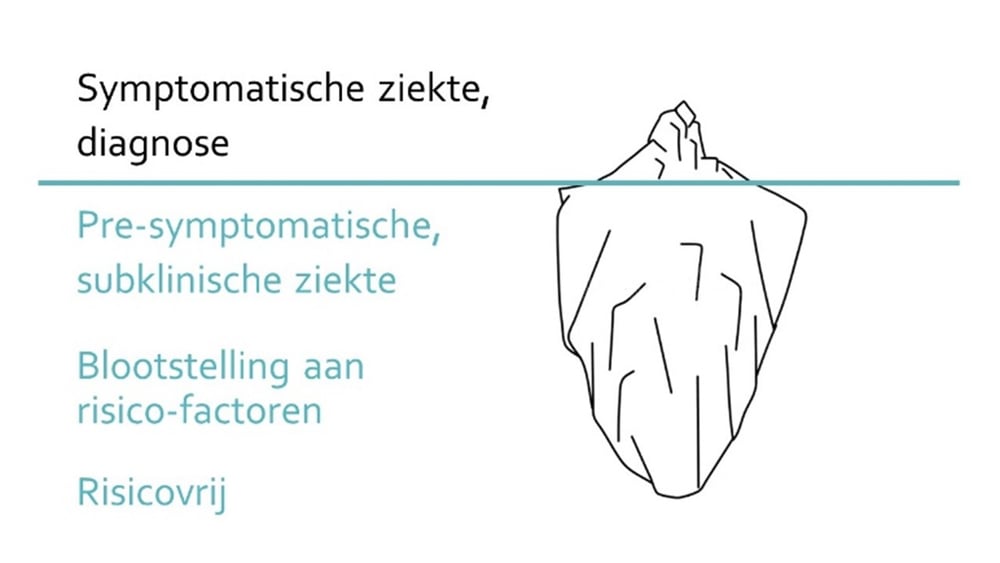
Prevention's role in the 'disease iceberg'
Curative care does not address this hidden part of the iceberg; this task falls to preventive health care. This part of care aims to protect, maintain and promote health [2,3]. A highly developed offer of cost-effective, preventive care can prevent the development of diseases as well as further complications in patients, thus allowing to avoid a loss of quality years of life. A quality and future-proof healthcare system thus has an interest in a good spread between preventive and curative healthcare. Despite this, only 2% of the total health budget in Belgium is invested in prevention [4].
The European average is around 3%. So while prevention across Europe remains a challenge, we are certainly not among the best in class [5]. This budget contrasts with the highly developed curative care system in our country, with a quality approach to acute syndromes thanks to high specialisation, freedom of choice and accessibility of care.
The intertwining of prevention and integrated care
Besides prevention, integrated care is also an important working point within our healthcare system; this is despite the introduction of some initiatives such as the Integrated Care Plan [6]. Integrated care implies that people experience continuity in care delivery: from health promotion and disease prevention, diagnosis and treatment, to disease management and palliative care. Preventive services also have an important role to play in this chain of healthcare providers. Thus, to achieve a successful and contemporary healthcare system, our preventive care needs to be strengthened and more closely intertwined with the curative aspect [7].
The impact on patients: the telling example of chronic diseases
The above shortcomings in terms of prevention and integrated care affect the patient. Indeed, healthcare providers from different disciplines cannot advise patients in a sufficiently coordinated manner. This is strongly reflected in the care of chronically ill patients; a category that will continue to pose a major challenge in the future. Diabetic patients, for example, often need a dietician, podiatrist and endocrinologist, but if these specialists only deal with their own care tasks, this leads to care fragmentation and, for example, potentially conflicting or incomplete treatment. To address this issue and encourage integrated care, the UZ Brussel, for example, opened Belgium's first integrated diabetes clinic in 2011.
Importance for primary care in the context of integrated care
The call for a different approach is not only heard from specialised care: primary care has also been calling for prevention and integrated care for some time. The recent reorganisation of the primary care in Flanders into primary care zones has as one of its objectives to strive for more integration and continuity of care [8]. This first line can therefore play an important role in this, which is expressed, for example, in care pathways [9]: a concept approach, treatment and follow-up of a patient (with a chronic condition) that is coordinated between patient, GP and specialist. A concrete example is the Type-2 diabetes care pathway in which the collaboration between patient, GP and specialist is formalised. Also for other conditions that require long-term follow-up, such as mental health conditions, such pathways can lead to care that is better coordinated between healthcare providers.
Adapted funding for a contemporary and future-proof healthcare system
Huisartsen gaven echter aan dat zij vaak onvoldoende tijd kunnen vrijmaken voor de preventieve opvolgingsactiviteiten van het HALT2Diabetes-programma [10]. Ondanks hun motivatie voor deze preventieve acties, worden ze enerzijds geconfronteerd met volle wachtkamers die acute zorg vragen en anderzijds met een financieringsmodel dat hen per prestatie vergoedt.
Besides the advantages of care pathways in terms of organisation and communication, this concept can also offer new insights in terms of financing: care pathways can be provided from bundled financing. Although such funding is not equally suitable for every condition or type of care and it also poses new challenges, it gives healthcare professionals an alternative to the current per-performance payment, also known as the fee-for-service system. From a prevention point of view, however, we are bumping up against the limits of this system which was illustrated, for example, during an evaluation of the Flemish HALT2Diabetes programme: an intensive lifestyle intervention programme for patients with Type-2 diabetes. Lifestyle interventions can be organised cost-effectively and have the potential to achieve sustainable behavioural change and thus prevent (further complications due to) diabetes in high-risk patients.
However, GPs indicated that they often cannot spare enough time for the preventive follow-up activities of the HALT2Diabetes programme [10]. Despite their motivation for these preventive actions, they are faced, on the one hand, with full waiting rooms demanding acute care and, on the other, with a funding model that reimburses them on a per-performance basis.
The role of prevention and integrated care in a future-proof healthcare system
In the examples above, we already see some great initiatives around prevention and integrated care in Belgium. What this still lacks is a coherent system in which prevention and integrated care are given the place they deserve based on their potential health gains. A look abroad may also provide some inspiration in this regard. In this way, we will hopefully arrive at a more central place for prevention that can bring the hidden part of the 'disease iceberg' more to the surface.
Would you like to know more about Désirée's doctoral research or would you like to coordinate with us about prevention and/or integrated care and how Möbius can support you in this? Feel free to contact us!
Sources
[1] Bhopal RS. (2002), Natural history, spectrum, iceberg, population patterns, and screening. Interrelated concepts in the epidemiology of disease. In: Concepts of Epidemiology: An Integrated Introduction to the Ideas, Theories, Principles and Methods of Epidemiology. New York: Oxford University Press; 133-161. URL: https://skums.ac.ir/dorsapax/userfiles/file/Epidemiology_Concepts_2002.pdf.
[2] AFMC (2013), AFMC Primer on Population Health. A virtual textbook on Public Health concepts for clinicians. URL: https://afmc.ca/medical-education/public-health.
[3] Vlaams Agentschap Zorg en Gezondheid (2018), Preventie. URL: https://www.zorg-en-gezondheid.be/preventie.
[4] WHO (2014), The case for investing in public health. URL: https://www.euro.who.int/__data/assets/pdf_file/0009/278073/Case-Investing-Public-Health.pdf
[5] Eurostat (2021), Health care expenditure by function, HLTH_SHA11_HC.
[6] KCE (2019), De performantie van het Belgische gezondheidssysteem, URL: https://kce.fgov.be/nl/de-performantie-van-het-belgische-gezondheidssysteem-%E2%80%93-rapport-2019
[7] WHO Regional Office for Europe (2016), The European Framework for Action on Integrated Health Services Delivery: an overview. Denmark: WHO Regional Office for Europe. URL: http://www.euro.who.int/en/health-topics/Health-systems/health-services-delivery/publications/2016/the-european-framework-for-action-on-integrated-health-services-delivery-an-overview-2016
[8] Vlaams Agentschap Zorg en Gezondheid (2017), Beleidsvisie: een geïntegreerde zorg in de eerste lijn. URL: https://www.zorg-en-gezondheid.be/sites/default/files/atoms/files/CELZ%20beleidstekst%20hervorming%20eerstelijnszorg.pdf
[9] RIZIV (2020), Zorgtrajecten.
[10] Van Hecke M., (2014), De lokale implementatie van een model voor vroegscreening, detectie en preventie van type 2 diabetes mellitus in de huisartsenpraktijk (binnen het HALT2Diabetes project).